Minimally Invasive Surgery
- Vaginal Hysterectomy
- Laparoscopic Hysterectomy
- Urinary Incontinence
- Pelvic Prolapse (Sagging Pelvic Organs)
- Laparoscopic Endometriosis Surgery
- Laparoscopic Fibroid Surgery (Myomectomy)
- Other Procedures
Minimally Invasive Surgery allows the surgeon to perform traditional procedures with small incisions on the abdominal wall.
Traditional surgery is performed through a large incision on the abdominal wall which permits visualization of and access to internal organs. Minimally Invasive Surgery allows the surgeon to perform these same procedures with small incisions on the abdominal wall. A small camera and telescopic surgical instruments are passed through these incisions. Some procedures are even done with no abdominal incision at all! Women who have had minimally invasive surgery are able to enjoy a shorter hospital stay, shorter recovery time, quicker return to work, and minimal scarring.
Minimally Invasive Surgery vs. Traditional surgery:
- Better cosmetic result- less scarring ( ¼ inch scars vs. 6-12 inch scar)
- Short hospital stay (4-23 hours vs. 3-4 days)
- Shorter recovery and faster return to work (10-14 days vs. 6-8 weeks)
- Minimal blood loss
- Less tissue trauma
- Less postoperative pain
More information on Minimally Invasive Surgery can been found at: www.hysterectomyoptions.com
Vaginal Hysterectomy
Vaginal hysterectomy is the least invasive of all as there are no incisions at all on the abdomen. This results in less pain and faster recovery. Not all patients are ideal candidates for vaginal surgery. For example if there is a cyst or tumor which must be evaluated the time, or if there is a history of scar tissue from prior surgeries then laparoscopy may be needed.
Laparoscopic Hysterectomy
Background:
The laparoscopic hysterectomy is a minimally invasive surgical alternative to the open abdominal hysterectomy. In the most recent hospital survey it was concluded that nearly 70% of hysterectomies done for benign (non-cancerous) indications are performed through the open abdominal method using a large vertical incision or a C-section scar. The open abdominal hysterectomy can be performed safely and effectively, and is currently the standard of care. However alternatives such as vaginal and laparoscopic hysterectomy are available. If you have been told that you are not a candidate for these procedures, you should seek a second opinion. In skilled hands, virtually any patient is a candidate for a minimally invasive hysterectomy regardless of the size and shape of the uterus, presence of endometriosis, or prior surgeries. The laparoscopic hysterectomy is an excellent alternative which offers all of the benefits of minimally invasive surgery.
Procedure:
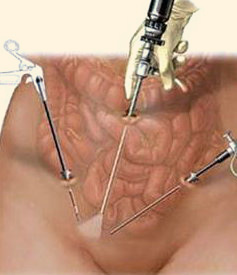
The Laparoscope is placed through a small incision in the umbilicus (belly button) to view the internal organs. The images of the operative field are displayed on an HD television screen. Then two other small incisions are made on the abdomen and are used to pass telescopic precision surgical instruments. The surgeon manipulates these laparoscopic instruments to complete the removal of the uterus using surgical dissection and energy devices. Depending on the indication, the procedure can be completed with or without removal of the cervix, tubes and ovaries. The procedure can be done on an outpatient basis, allowing the patient to have a hysterectomy without spending a single night in the hospital.
Update:
The newest advance in surgical technology uses the Robotic (da Vinci) Hysterectomy procedure.
Urinary Incontinence
Background:
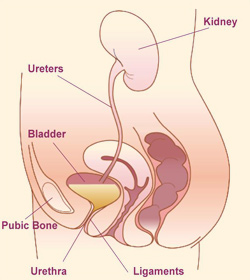
Many women suffer from Urinary Incontinence. At first a woman may only experience an occasional leakage of urine with a cough or a sudden urge to run to the bathroom. However, over time it can develop into a chronic and constant problem that alters her way of life. Frequently she will give up activities such as exercise, or will require a sanitary pad to prevent accidents whenever she leaves the house. Many women refuse to discuss Urinary Incontinence due to feelings of embarrassment, and simply consider these 'accidents' to be a normal part of aging. In reality urinary incontinence is NOT a normal part of the aging process. It is a very common medical problem. In fact 33% of women over the age of 65 suffer with this condition. However urinary incontinence can also affect younger women as well. Fortunately, very effective treatment options exist. There are several different causes of urinary incontinence, and treatments can involve conservative therapy, exercises, biofeedback, medical therapy, and surgery.
Procedure:
Dr. Hunter uses office urodynamic testing to identify the underlying causes for the urinary incontinence. She offers the latest Minimally Invasive treatment options. For a woman with Stress Unrinary Incontinence, Dr. Hunter offers a simple outpatient surgical treatment which can permanently prevent leakage, and restore her quality of life. The treatment involves the placement of a bladder sling with tiny visible incisions. This suburethral sling is performed in the operating room in under an hour.
Pelvic Prolapse (Sagging Pelvic Organs)
Background:
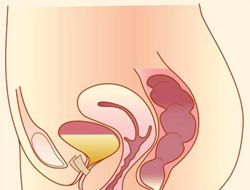
Pelvic floor defects can occur for many reasons. Common causes include the vaginal delivery of a large infant, or the tissue trauma resulting from a prolonged labor process. Over time tissue weakness in the pelvic floor can result in the prolapse sagging of the uterus, bladder, or rectum to the level of the vaginal opening or beyond. In severe cases the entire uterus and vagina can appear as a large mass completely protruding out of the vaginal opening. Common symptoms of prolapse include pelvic pain and pressure, low back pain, sexual pain, frequent urination, incomplete bladder emptying, constipation, and vaginal bleeding.
Procedure:
Many treatment options exist including pelvic floor exercise, pessary placement, and surgical repair. Dr Hunter offers all of these therapies including vaginal pelvic reconstruction. She is trained in all forms of pelvic support surgery including anterior/posterior repair, perineorrhaphy, suburethral sling, barchype unethopexy, para vaginal defect repair, sacrospinous fixation, uterosacral ligament suspension, and open or laparoscopic sacrocolpopexy. Hunter Women's Clinic is a referral practice for evaluating and treating complicated degrees of prolapse. In some cases of recurrent prolapse, laparoscopic sacral-colpopexy is required. This procedure has a very high success rate and is considered the 'gold standard' for apical prolapse. However it is a very intricate procedure, and physicians must have advanced training to become proficient. The top of the vagina is supported by a synthetic mesh material. This mesh is then affixed to the strong and durable sacral anterior longitudinal fascia.
Laparoscopic Endometriosis Surgery
Background:
There are many causes of chronic and severe menstrual pelvic pain. Endometriosis is a condition that involves the abnormal growth of uterine menstrual tissue inside the abdomen and pelvis. This condition can cause severe menstrual pain which can interrupt daily activities and require a woman to take time off of work. In extreme cases it can leave her incapacitated for 5-10 days of the month. Endometriosis can also cause sexual pain, difficulties urinating, and bowel irregularity. The treatment of endometriosis can be challenging. Many medical treatments exist, however they are often inadequate, short term, and can not be used in a woman who is trying to become pregnant.
Procedure:
Dr. Hunter offers laparoscopic excision of endometriosis. She uses advanced surgical dissection techniques to remove all of the pelvic tissue which contains the endometriosis implants. The result for most women is a significant improvement or resolution of pain symptoms, and enhanced fertility.
Laparoscopic Fibroid Surgery (Myomectomy)
Background:
Uterine Fibroids are the most common benign tumor found in the female reproductive tract. They are found in 20-40% of women. Fibroid tumors are caused by a localized overgrowth of muscle fibers which start out as microscopic tumors. Most fibroids range in size from a marble to a grapefruit. However in extreme cases they can grow immensely and distend the abdomen to the size of a full term pregnancy. Fibroids can present in various ways, and women may complain of any of the following symptoms: heavy vaginal bleeding, pelvic pressure, pelvic pain, constipation, sexual discomfort, urinary frequency, abdominal swelling, and infertility. Complications of fibroids include: heavy irregular vaginal bleeding, anemia, blood transfusion, recurrent miscarriages, and severe pain.
Procedure:
At Hunter Women's Clinic, fibroid tumors are diagnosed by patient symptoms, family history, pelvic exam, and ultrasound. MRI may also be used. Fibroid tumors constitute the most common indication for hysterectomy in the United States. However many women with fibroids desire to maintain their fertility options. For these women Dr. Hunter offers laparoscopic and Robotic Myomectomy. This procedure is performed though small incisions and involves the removal of fibroids while preserving the uterus and the patient's fertility. The patient is often able to return home the same day of surgery.
Other minimally invasive surgical procedures in gynecology
In addition to the specific conditions listed above, Dr. Hunter offers a minimally invasive alternative for every surgical procedure that can be done in gynecology. Examples include Fibroid surgery (myomectomy), removal of ovarian cysts and tumors, removal of one or both tubes and/or ovaries, infertility surgery of the fallopian tubes, ectopic pregnancy, pelvic support surgery (Sacral-colpopexy), and pelvic pain surgery. Dr. Hunter also performs minimally invasive infertility surgery including surgical correction of a damaged fallopian tube (Neosalpingostomy).
